The US Preventive Services Task Force (USPSTF) issued an update to its colorectal cancer (CRC) screening guideline that includes a recommendation lowering the age at which to start screening US adults at average risk from the current recommendation of age 50 to age 45. The new recommendation matches that of the American Cancer Society. Average risk is defined as no prior diagnosis of CRC, adenomatous polyps, or inflammatory bowel disease, and no personal diagnosis or family history of known genetic disorders that predispose to a high lifetime risk of CRC (such as Lynch syndrome or familial adenomatous polyposis).
The USPSTF cited evidence of increased incidence of CRC in people younger than age 50—10.5% of new CRC cases occur in persons younger than 50 years. Incidence of CRC (specifically adenocarcinoma) in adults aged 40 to 49 years has increased by almost 15% from 2000-2002 to 2014-2016. Starting CRC screening at age 45 years may moderately increase life-years gained and decrease CRC cases and deaths compared with beginning screening at age 50. Rates of CRC incidence are higher in Black adults and American Indian and Alaska Native adults, persons with a family history of CRC (even in the absence of any known inherited syndrome), men, and persons with other risk factors such as obesity, diabetes, and long-term smoking and unhealthy alcohol use. All adults 45 years or older should be offered screening, even if these risk factors are absent. However, in adults 86 years or older, evidence on benefits and harms of CRC screening is lacking, and competing causes of mortality likely preclude any survival benefit that would outweigh the harms of screening, the recommendation states.
The USPSTF continues to conclude with high certainty that screening for CRC in adults aged 50 to 75 years has substantial net benefit, but has now added the conclusion with moderate certainty that screening for CRC in adults aged 45 to 49 years has moderate net benefit. For adults aged 76 to 85 years who have been previously screened, the USPSTF states with moderate certainty that CRC screening has only small benefit; however, those who have never been screened for CRC are more likely to benefit.
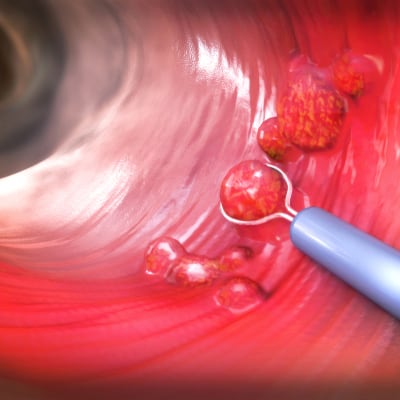
Recommended screening strategies include:
- High-sensitivity guaiac fecal occult blood test (HSgFOBT) or fecal immunochemical test (FIT) every year
- Stool DNA-FIT every 1 to 3 years
- Computed tomography colonography every 5 years
- Flexible sigmoidoscopy every 5 years
- Flexible sigmoidoscopy every 10 years + annual FIT
- Colonoscopy screening every 10 years
The tests require different frequencies of screening, location of screening, methods of screening, pre-procedure bowel preparation, anesthesia or sedation during the test, and follow-up procedures for abnormal findings. Discuss with patients the decision to screen, taking into consideration the patient’s overall health status (life expectancy, comorbid conditions), prior screening history, and preferences.